A Patient Who Has Received a Maximum Dose of Nitroglycerin Continues to Report Chest Pain
Treatment of acute coronary syndromes Overview of Acute Coronary Syndromes (ACS) Acute coronary syndromes result from acute obstruction of a coronary artery. Consequences depend on degree and location of obstruction and range from unstable angina to non–ST-segment elevation... read more (ACS) is designed to relieve distress, interrupt thrombosis, reverse ischemia, limit infarct size, reduce cardiac workload, and prevent and treat complications. An ACS is a medical emergency; outcome is greatly influenced by rapid diagnosis and treatment. Treatment occurs simultaneously with diagnosis. Treatment includes revascularization Revascularization for Acute Coronary Syndromes Revascularization is the restoration of blood supply to ischemic myocardium in an effort to limit ongoing damage, reduce ventricular irritability, and improve short-term and long-term outcomes... read more (with percutaneous coronary intervention Percutaneous Coronary Interventions (PCI) Percutaneous coronary interventions (PCI) include percutaneous transluminal coronary angioplasty (PTCA) with or without stent insertion. Primary indications are treatment of Angina pectoris... read more  , coronary artery bypass grafting Coronary Artery Bypass Grafting (CABG) Frontal and lateral chest x-ray of a patient post coronary artery bypass surgery showing sternal sutures (black arrow) and surgical clips (red arrow). Coronary artery bypass grafting (CABG)... read more
, coronary artery bypass grafting Coronary Artery Bypass Grafting (CABG) Frontal and lateral chest x-ray of a patient post coronary artery bypass surgery showing sternal sutures (black arrow) and surgical clips (red arrow). Coronary artery bypass grafting (CABG)... read more  , or fibrinolytic therapy) and drug therapy to treat ACS and underlying coronary artery disease Overview of Coronary Artery Disease Coronary artery disease (CAD) involves impairment of blood flow through the coronary arteries, most commonly by atheromas. Clinical presentations include silent ischemia, angina pectoris, acute... read more
, or fibrinolytic therapy) and drug therapy to treat ACS and underlying coronary artery disease Overview of Coronary Artery Disease Coronary artery disease (CAD) involves impairment of blood flow through the coronary arteries, most commonly by atheromas. Clinical presentations include silent ischemia, angina pectoris, acute... read more 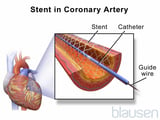 .
.
Drugs used depend on the type of ACS and include
-
Aspirin, clopidogrel, or both (prasugrel or ticagrelor are alternatives to clopidogrel if fibrinolytic therapy has not been given)
-
Beta-blocker
-
Glycoprotein IIb/IIIa inhibitor considered for certain patients undergoing percutaneous coronary intervention (PCI) and high risk lesions (eg, high thrombus burden, no reflow)
-
Fibrinolytics for select patients with STEMI when timely PCI unavailable
-
Angiotensin-converting enzyme (ACE) inhibitor (as early as possible)
-
Statins
Antiplatelet and antithrombotic drugs, which stop clots from forming, are used routinely. Anti-ischemic drugs (eg, beta-blockers, IV nitroglycerin) are frequently added, particularly when chest pain or hypertension is present (see table Drugs for Coronary Artery Disease Drugs for Coronary Artery Disease* ![]() ).
).
Chest pain can be treated with nitroglycerin or sometimes morphine. Nitroglycerin is preferable to morphine, which should be used judiciously (eg, if a patient has a contraindication to nitroglycerin or is in pain despite nitroglycerin therapy). Nitroglycerin Nitrates Treatment of acute coronary syndromes (ACS) is designed to relieve distress, interrupt thrombosis, reverse ischemia, limit infarct size, reduce cardiac workload, and prevent and treat complications... read more is initially given sublingually, followed by continuous IV drip if needed. Morphine 2 to 4 mg IV, repeated every 15 minutes as needed, is highly effective but can depress respiration, can reduce myocardial contractility, and is a potent venous vasodilator. Evidence also suggests that morphine interferes with some P2Y12 receptor inhibitors. A large retrospective trial showed that morphine may increase mortality in patients with acute myocardial infarction (1, 2 References Treatment of acute coronary syndromes (ACS) is designed to relieve distress, interrupt thrombosis, reverse ischemia, limit infarct size, reduce cardiac workload, and prevent and treat complications... read more ). Hypotension and bradycardia secondary to morphine can usually be overcome by prompt elevation of the lower extremities.
-
1. Meine TJ, Roe MT, Chen AY, et al: Association of intravenous morphine use and outcomes in acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. Am Heart J 149(6):1043-1049, 2005. doi 10.1016/j.ahj.2005.02.010
-
2. Kubica J, Adamski P, Ostrowska M, et al: Morphine delays and attenuates ticagrelor exposure and action in patients with myocardial infarction: the randomized, double-blind, placebo-controlled IMPRESSION trial. Eur Heart J 37(3):245–252, 2016. doi: 10.1093/eurheartj/ehv547
Aspirin, clopidogrel, prasugrel, ticagrelor, ticlopidine, and glycoprotein (GP) IIb/IIIa inhibitors are examples of antiplatelet drugs. All patients are given aspirin 160 to 325 mg (not enteric-coated), if not contraindicated (eg, life-threatening active bleeding), at presentation and 81 mg once a day indefinitely thereafter. Chewing the first dose before swallowing quickens absorption. Aspirin reduces short- and long-term mortality risk (1 Antiplatelet drug references Treatment of acute coronary syndromes (ACS) is designed to relieve distress, interrupt thrombosis, reverse ischemia, limit infarct size, reduce cardiac workload, and prevent and treat complications... read more ).
If aspirin cannot be taken, clopidogrel 75 mg orally once a day or ticlopidine 250 mg orally twice a day may be used. Clopidogrel has largely replaced ticlopidine for routine use because neutropenia is a risk with ticlopidine and the white blood cell count must be monitored regularly.
In patients undergoing PCI Revascularization for Acute Coronary Syndromes Revascularization is the restoration of blood supply to ischemic myocardium in an effort to limit ongoing damage, reduce ventricular irritability, and improve short-term and long-term outcomes... read more , a loading dose of clopidogrel (300 to 600 mg orally once), prasugrel (60 mg orally once), or ticagrelor (180 mg orally once) improves outcomes (2 Antiplatelet drug references Treatment of acute coronary syndromes (ACS) is designed to relieve distress, interrupt thrombosis, reverse ischemia, limit infarct size, reduce cardiac workload, and prevent and treat complications... read more ).
Some clinicians give a GP IIb/IIIa inhibitor during PCI to all high-risk patients (eg, those with markedly elevated cardiac markers, a TIMI risk score ≥ 4, or persistent symptoms despite adequate drug therapy) with large thrombus burden. The GP IIb/IIIa inhibitor is continued for 6 to 24 hours, and angiography is done before the infusion period is over. GP IIb/IIIa inhibitors are not recommended for patients receiving fibrinolytics. Abciximab, tirofiban, and eptifibatide appear to have equivalent efficacy, and the choice of drug should depend on other factors (eg, cost, availability, familiarity).
For patients receiving a stent for revascularization, aspirin is continued indefinitely. Clopidogrel 75 mg orally once a day, prasugrel 10 mg orally once a day, or ticagrelor 90 mg orally twice a day should be used for at least 1 month in patients with a bare-metal stent. Patients with a drug-eluting stent after ACS have a prolonged risk of thrombosis and benefit from at least 12 months of clopidogrel (or prasugrel or ticagrelor) treatment.
-
1. Levine GN, Bates ER, Bittl JA, et al: 2016 ACC/AHA Guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. J Am Coll Cardiol 68 (10): 1082–115, 2016.
-
2. Lawton JS, Tamis-Holland JE, Bangalore S, et al: 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the ACC/AHA Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 79(2):e21–e129, 2022. doi: 10.1016/j.jacc.2021.09.006
Either a low molecular weight heparin (LMWH), unfractionated heparin, or bivalirudin is given routinely to patients with acute coronary syndrome unless contraindicated (eg, by active bleeding or planned use of streptokinase or anistreplase). Choice of agent is somewhat involved.
Patients at high risk of systemic emboli (eg, atrial fibrillation with CHA2DS2VASc score CHA2DS2-VASc Score ![]() ≥ 2) also require long-term therapy with an oral anticoagulant (eg, warfarin, dabigatran, apixaban, rivaroxaban). Conversion to oral anticoagulants should begin 48 hours after symptom resolution or PCI.
≥ 2) also require long-term therapy with an oral anticoagulant (eg, warfarin, dabigatran, apixaban, rivaroxaban). Conversion to oral anticoagulants should begin 48 hours after symptom resolution or PCI.
Unfractionated heparin is more complicated to use because it requires frequent (every 6 hours) dosing adjustments to achieve an activated partial thromboplastin time (aPTT) 1.5 to 2 times the control value. In patients undergoing angiography, further dosing adjustment is done to achieve an activated clotting time (ACT) of 200 to 250 seconds if the patient is treated with a GP IIb/IIIa inhibitor and 250 to 300 seconds if a GP IIb/IIIa inhibitor is not being given. However, if bleeding develops after catheterization, the effects of unfractionated heparin are shorter and can be reversed (by promptly stopping the heparin infusion and giving protamine sulfate).
The LMWHs have better bioavailability, are given by simple weight-based dose without monitoring aPTT and dose titration, and have lower risk of heparin-induced thrombocytopenia. They also may produce an incremental benefit in outcomes relative to unfractionated heparin in patients with ACS. Of the LMWHs, enoxaparin appears to be superior to dalteparin or nadroparin. However, enoxaparin may pose a higher bleeding risk in patients with STEMI who are > 75, and its effects are not completely reversible with protamine.
Thus, taking all into account, many published guidelines recommend LMWH (eg, enoxaparin) over unfractionated heparin in patients with unstable angina or NSTEMI and in patients < age 75 with STEMI who are not undergoing PCI.
By contrast, unfractionated heparin is recommended when emergency PCI is done (eg, patients with acute STEMI who proceed to the catheterization laboratory), when CABG is indicated within the next 24 hours, and when patients are at high risk of bleeding complications (eg, history of gastrointestinal bleeding within the last 6 months) or have creatinine clearance < 30 mL/minute. Ongoing studies should help clarify the choice between LMWH and unfractionated heparin.
For patients undergoing PCI, post-procedure heparin is no longer recommended unless patients are at high risk of thromboembolic events (eg, patients with large anterior MI, known LV thrombus, atrial fibrillation), because postprocedure ischemic events have decreased with the use of stents and antiplatelet drugs. For patients not undergoing PCI, heparin is continued for 48 hours (or longer if symptoms persist).
The direct thrombin inhibitors, bivalirudin and argatroban, may have a lower incidence of serious bleeding and improved outcomes, particularly in patients with renal insufficiency (hirudin, another direct thrombin inhibitor, appears to cause more bleeding than the other drugs). The factor Xa inhibitor, fondaparinux, reduces mortality and reinfarction in patients with NSTEMI who undergo PCI without increasing bleeding but may result in worse outcomes than unfractionated heparin in patients with STEMI. Although routine use of these alternative anticoagulants is thus not currently recommended, they should be used in place of unfractionated heparin or LMWH in patients with a known or suspected history of heparin-induced thrombocytopenia.
Bivalirudin is an acceptable anticoagulant for patients undergoing primary PCI who are at high risk of bleeding and is recommended for those with a known or suspected history of heparin-induced thrombocytopenia. For patients with unstable angina or NSTEMI, dose is an initial bolus of 0.1 mg/kg IV followed by a drip of 0.25 mg/kg/hour. For patients with STEMI, initial dose is 0.75 mg/kg IV followed by 1.75 mg/kg/hour.
These drugs are recommended unless contraindicated (eg, by bradycardia, heart block Atrioventricular Block Atrioventricular (AV) block is partial or complete interruption of impulse transmission from the atria to the ventricles. The most common cause is idiopathic fibrosis and sclerosis of the conduction... read more 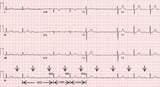 , hypotension, or asthma Asthma Asthma is a disease of diffuse airway inflammation caused by a variety of triggering stimuli resulting in partially or completely reversible bronchoconstriction. Symptoms and signs include dyspnea... read more ), especially for high-risk patients. Beta-blockers reduce heart rate, arterial pressure, and contractility, thereby reducing cardiac workload and oxygen demand. Infarct size largely determines cardiac performance after recovery. Oral beta-blockers given within the first few hours improve prognosis by reducing infarct size, recurrence rate, incidence of ventricular fibrillation, and mortality risk (1 Beta-blocker reference Treatment of acute coronary syndromes (ACS) is designed to relieve distress, interrupt thrombosis, reverse ischemia, limit infarct size, reduce cardiac workload, and prevent and treat complications... read more ).
, hypotension, or asthma Asthma Asthma is a disease of diffuse airway inflammation caused by a variety of triggering stimuli resulting in partially or completely reversible bronchoconstriction. Symptoms and signs include dyspnea... read more ), especially for high-risk patients. Beta-blockers reduce heart rate, arterial pressure, and contractility, thereby reducing cardiac workload and oxygen demand. Infarct size largely determines cardiac performance after recovery. Oral beta-blockers given within the first few hours improve prognosis by reducing infarct size, recurrence rate, incidence of ventricular fibrillation, and mortality risk (1 Beta-blocker reference Treatment of acute coronary syndromes (ACS) is designed to relieve distress, interrupt thrombosis, reverse ischemia, limit infarct size, reduce cardiac workload, and prevent and treat complications... read more ).
Heart rate and BP must be carefully monitored during treatment with beta-blockers. Dosage is reduced if bradycardia or hypotension develops. Excessive adverse effects may be reversed by infusion of the beta-adrenergic agonist isoproterenol 1 to 5 mcg/minute.
-
1. Chen ZM, Pan HC, Chen YP, et al. Early intravenous then oral metoprolol in 45,852 patients with acute myocardial infarction: randomised placebo controlled trial. Lancet 366:1622–1632, 2005.
A short-acting nitrate, nitroglycerin, is used to reduce cardiac workload in selected patients. Nitroglycerin dilates veins, arteries, and arterioles, reducing left ventricular preload and afterload. As a result, myocardial oxygen demand is reduced, lessening ischemia.
Longer use may benefit patients with recurrent chest pain or persistent pulmonary congestion. In high-risk patients, nitroglycerin given in the first few hours reduces infarct size and short-term and possibly long-term mortality risk. Nitroglycerin is not routinely given to low-risk patients with uncomplicated myocardial infarction.
Tenecteplase (TNK), alteplase (rTPA), reteplase (rPA), streptokinase, and anistreplase (anisoylated plasminogen activator complex—APSAC), all given IV, are plasminogen activators. They convert single-chain plasminogen to double-chain plasminogen, which has fibrinolytic activity. They have different characteristics and dosing regimens (see table IV Fibrinolytic Drugs IV Fibrinolytic Drugs ![]() ) and are appropriate only for selected patients with STEMI Infarct extent
) and are appropriate only for selected patients with STEMI Infarct extent  ).
).
Tenecteplase and reteplase are recommended most often because of their simplicity of administration; tenecteplase is given as a single bolus over 5 seconds and reteplase as a double bolus 30 minutes apart. Administration time and drug errors are reduced compared with other fibrinolytics. Tenecteplase, like alteplase, has an intermediate risk of intracranial hemorrhage, has a higher rate of recanalization than other fibrinolytics, and is expensive. Reteplase has the highest risk of intracranial hemorrhage and a recanalization rate similar to that of tenecteplase, and it is expensive.
Streptokinase (currently not available in the US) may induce allergic reactions, especially if it has been used previously, and must be given by infusion over 30 to 60 minutes; however, it has a low incidence of intracerebral hemorrhage and is relatively inexpensive. Anistreplase, related to streptokinase, is similarly allergenic and slightly more expensive but can be given as a single bolus. Neither drug requires concomitant heparin use. For both, recanalization rate is lower than that with other plasminogen activators. Because of the possibility of allergic reactions, patients who previously received streptokinase or anistreplase are not given that drug again.
Alteplase is given in an accelerated or front-loaded dosage over 90 minutes. Alteplase with concomitant IV heparin improves patency, is nonallergenic, and has a higher recanalization rate than other fibrinolytics.
There are many absolute and relative contraindications to fibrinolytic therapy. In general, the presence of active bleeding or a condition where bleeding would be life-threatening is an absolute contraindication. The contraindications to fibrinolytic therapy are listed in the table Contraindications to Fibrinolytic Therapy Contraindications to Fibrinolytic Therapy ![]() .
.
Angiotensin-converting enzyme (ACE) inhibitors reduce mortality risk in patients with myocardial infarction, especially in those with anterior infarction, heart failure, or tachycardia. The greatest benefit occurs in the highest-risk patients early during convalescence. ACE inhibitors are given > 24 hours after thrombolysis stabilization and, because of continued beneficial effect, may be prescribed long-term.
Angiotensin II receptor blockers (ARBs) may be an effective alternative for patients who cannot tolerate ACE inhibitors (eg, because of cough). Currently, they are not first-line treatment after myocardial infarction. Contraindications include hypotension, kidney failure, bilateral renal artery stenosis, and known allergy.
Statins (HMG-CoA reductase inhibitors) have long been used for prevention of coronary artery disease and ACS, but there is now increasing evidence that they also have short-term benefits, such as stabilizing plaque, reversing endothelial dysfunction, decreasing thrombogenicity, and reducing inflammation. Thus, all patients without contraindications (eg, statin-induced myopathy, liver dysfunction) to therapy should receive a statin at the maximally tolerated dose as early as possible following ACS regardless of their serum lipid levels.
PCSK-9 inhibitors (evolocumab, alirocumab) are used for patients not at target LDL-C levels. They are used alone or in combination with other lipid-lowering therapies (eg, statins, ezetimibe) for the treatment of adults with primary hyperlipidemia (including familial hypercholesterolemia).
Source: https://www.msdmanuals.com/professional/cardiovascular-disorders/coronary-artery-disease/drugs-for-acute-coronary-syndromes
0 Response to "A Patient Who Has Received a Maximum Dose of Nitroglycerin Continues to Report Chest Pain"
Post a Comment